48 YEAR OLD WOMEN WITH MULTI-SYSTEM INVOLVEMENT.
CBBLE UDHC SIMILAR CASES
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box .
48 year old female , resident of Hyderabad and home -maker by occupation, presented to casualty on 14/3/22 with complaints of ,
SHORTNESS OF BREATH since 1 week - initially grade -2 later progressed to grade 4 .
PEDAL EDEMA since 1 week
CHEST TIGHTNESS since 1 week
GENERALISED WEAKNESS AND FATIGUE AND FREQUENT FALLS since 1 week
DIFFICULTY OPENING MOUTH AND ORAL ULCERS since 1 week.
DIFFICULTY IN SWALLOWING BOTH SOLIDS AND LIQUIDS since 3 days .
H/O SKIN PEELING ALL OVER BODY 25 DAYS ago .
HOPI :
PT HUSBAND - AUTO-DRIVER .
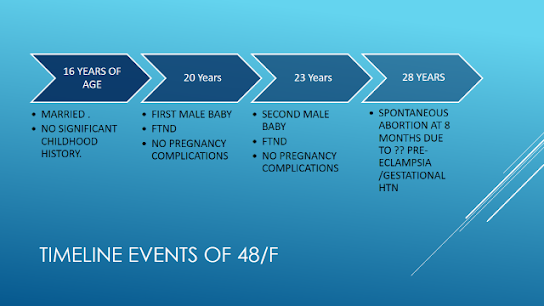
TIMELINE :
25- JAN 2022 :
PERSONAL HISTORY :
LOSS OF APPETITE
WEIGHT LOSS PRESENT
SLEEP ADEQUATE
BOWEL AND BLADDER MOVEMENTS REGULAR
C/O BURNING MICTURATION SINCE 1 WEEK
GENERAL EXAMINATION :
PT C/C/C
PALLOR - PRESENT
NO ICTERUS ,CYANOSIS ,CLUBBING ,LYMPHADENOPATHY
MILD EDEMA - NON PITTING EXTENDING UPTO FEET .
VITALS ON ADMISSION :
ALOPECIA- PRESENT.
EYES - PROPTOSIS SEEN . NO CONJUNCTIVAL SUFFUSION
EOM- INTACT
MICROSTOMIA PRESENT
BALD TONGUE NOTED . RED COLOR
NO ULCERS .
THYROID- NO GOITRE NOTED
SKIN -
MULTIPLE HYPER- PIGMENTED MACULES SEEN ALL OVER FACE, UPPER LIMBS , NECK ,THIGH , ABDOMEN AND UPPER BACK .
DRY SKIN PRESENT
THICKENING OF SKIN NOTED OVER FORE ARMS , DORSUM OF HAND AND FINGERS AND ON AROUND MOUTH.
ABSENT HAIR
SLIGHT PEELING STILL NOTED OVER ARMS AND LEGS .
SYSTEMIC EXAMINATION :
https://youtube.com/shorts/GiZhR3TUUM0?feature=share
Probable reason for less predominant /decreased frequency of RAYNAUDS PHENOMENON now compared to previously may be because of concomitant usuage of calcium channel blockers (Amlodipine for HTN )
FINAL DIAGNOSIS :
CONNECTIVE TISSUE DISORDER - ? LIMITED SYSTEMIC SCLEROSIS .
? MCTD
( IN BACKGROUND OF RAYNAUDS PHENOMENON , POLYARTHRITIS , SKIN THICKENING and MICROSTOMIA , DIFFICULTY SWALLOWING , ?? ILD / PROTEINURIA . )
? ERYTHRODERMA ( secondary to ?? ISONIAZIDE ) - RESOLVED .
K/C/O HTN , DM- 2 and HYPOTHYROIDISM .
Anemia of chronic disease
Credits : Special thanks to Dr Phaneendra (intern ) and Dr .V. Pavan kalyan(intern) for clinical images .
- DIAGNOSTIC UNCERTAINTIES :
1) Does our patient have ILD or Miliary tuberculosis ?
A) Going with long standing history of fatigue ,weight loss , polyarthralgia ,alopecia and raynauds . Our first differential was ILD .
SO Repeat HRCT was planned .
Sputum AFB repeated was negative . Previously also sputum CBNAAT was negative .
But we have to be sure about the diagnosis as treatment for both are completely opposite .
-Steroids would be the treatment for her underlying scleroderma/ILD . But can aggrevate her underlying tuberculosis if at all she has one
- Empirical ATT is also not advisable,as she had developed intense drug reaction previously, which could be fatal .
So currently we are trying to evaluate her by repeating HRCT and looking at progression/regression .
Plan for bronchoscopy and BAL for CBNAAT ( Sensitivity is again low especially if it's miliary tuberculosis ) .
- Planning to send ANA profile also .( Anti- centromere,anti scl-70 ,anti Rna polymerase antibodies )
2) Sensitivity of nail fold capillaroscopy in diagnosis of secondary raynauds ?
A) Nailfold capillaroscopy is a useful tool to distinguish primary from secondary Raynaud's phenomenon (RP) by examining the morphology of nailfold capillaries.
P- The data between the year 2005 and 2009 were retrieved from the nailfold capillaroscopic database of National Taiwan University Hospital (NTUH). Only the data from the patients with RP were analyzed.
O - The data from a total of 67 patients were qualified for the current study. We found the sensitivity and specificity of scleroderma pattern for systemic sclerosis (SSc) were 89.47% and 80%, and the specificity of the early, active, and late scleroderma patterns for SSc reached 87.5%, 97.5%, and 95%, respectively.
The nailfold capillaroscopic (NC) patterns may be useful in the differential diagnosis of CTDs with RP.
https://pubmed.ncbi.nlm.nih.gov/24016612/
23/3/22 :
Repeat HRCT :
Repeat HRCT showed decreased infiltration. So patient is probably responding to ATT.
BAL was done - NEGATIVE for AFB.
As clinical improvement and radiological improvement was present with ATT. With suspicion of miliary tuberculosis ,pt was restarted slowly on ATT under observation .
24 hour urine protein - 312 mg/day
24 hour urine creatinine -0.7 mg/ day
Ratio - 0.44
ANA PROFILE :
FINAL DIAGNOSIS :
1) MCTD ( raynauds positive; Anti sn RNP positive)
2) ? Miliary tuberculosis
3) HFREF secondary to ? CAD
4) HTN/ DM / HYPOTHYROIDISM.
5) Proteinuria
6) Anemia of chronic disease .
H/o ERYTHRODERMA secondary to ATT-
resolved .
DISCUSSION :
- PATHOPHYSIOLOGY OF SYSTEMIC SCLEROSIS :
https://musculoskeletalkey.com/etiology-and-pathogenesis-of-scleroderma/
https://plasticsurgerykey.com/systemic-sclerosis-scleroderma-and-related-disorders/
Patient was started on ATT , in view of suspicion of miliary tuberculosis - she developed intense rash and peeling of skin (ERYTHRODERMA/SJS) 20-25 days after Starting ATT.
Probably ?? isoniazide induced
- ERYTHRODERMA - ISONIAZIDE INDUCED :
Tuberculosis is a common infectious disease in developing countries. Isoniazid is established the first-line antitubercular drug and an essential component of all antitubercular regimens. Erythroderma caused by isoniazid is an uncommon but serious adverse drug reaction. We report here a case of a 63-year-old female patient who presented with generalized redness and scaling with itching after 8 weeks of antitubercular treatment (ATT).
- MANAGEMENT OF RAYNAUDS :
https://www.researchgate.net/figure/Treatment-algorithm-for-Raynauds-phenomenon_fig2_43227518









































Comments
Post a Comment