FEBRUARY BIMONTHLY ASSESSMENT
Medicine paper for February 2021 bimonthly blended assessment .
Here is link to question paper :
Questions :
1) Please go through the patient data in the links below and answer the following questions:
50 year man, he presented with the complaints of
Frequently walking into objects along with frequent falls since 1.5 years
Drooping of eyelids since 1.5 years
Involuntary movements of hands since 1.5 years
Talking to self since 1.5 years
More here: https://archanareddy07.blogspot.com/2021/02/50m-with-parkinsonism.html?m=1
Case presentation links:
https://youtu.be/kMrD662wRIQ
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
A ) 50 year old man, k/c/o diabetic since 9 months , presented with the complaints of:
Frequently walking into objects along with frequent falls since 1.5 years
Drooping of eyelids since 1.5 years
Involuntary movements of hands since 1.5 years
Talking to self since 1.5 years
Bed wetting since 1 year
With all these complaints a diagnosis of neuro degenerative disorder known as Progressive supranuclear palsy was suspected.
ANATOMICAL LOCALIZATION TO HIS PROBLEMS:
The anatomical localization to his problems appears to be in the brain
The anatomical location is in the Basal ganglia and substantia nigra.
Isolated dysfunction of vertical eye movements is due to a midbrain lesion affecting the rostral interstitial nucleus of the medial longitudinal fascicle, with impaired vertical saccades only, the interstitial nucleus of Cajal or the posterior commissure; common causes with an acute onset are an infarction or bleeding in the upper midbrain or in patients with chronic progressive supranuclear palsy (PSP) and Niemann-Pick disease.
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
A) ETIOLOGY - PROGRESSIVE SUPRANUCLEAR PALSY.
Progressive Supranuclear Palsy PSP is a neurodegenerative disease of unknown etiology in which neurons in the basal ganglia and brainstem degenerate. Clinical signs include downgaze palsy, loss of balance with backward falls, muscle rigidity, dysphagia, dysarthria, emotional lability (pseudobulbar palsy), mild dementia and resting tremor.A characteristic sign for PSP is the “round the houses” sign where vertical saccades follow a curved course due to inability to produce pure midline movement. Although Parkinson’s disease (PD) and PSP share several clinical features, downgaze palsy is not seen in PD and should lead clinicians to consider the diagnosis of PSP. The lesion is located above the cranial nerve nuclei that control vertical gaze, thus the name “supranuclear.”
SEQUENCE OF EVENTS :
c) What is the efficacy of each of the drugs listed in his current treatment plan
A) The patient was put on Syndopa
Quetiapine
A randomized, double-blind, placebo-controlled trial, we evaluated 361 patients with early Parkinson's disease who were assigned to receive carbidopa–levodopa at a daily dose of 37.5 and 150 mg, 75 and 300 mg, or 150 and 600 mg, respectively, or a matching placebo for a period of 40 weeks, and then to undergo withdrawal of treatment for 2 weeks
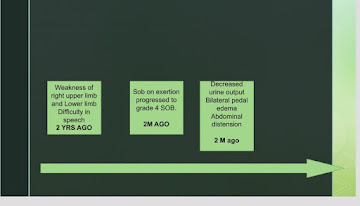
2) Patient was apparently asymptomatic 2 years back then he developed weakness in the right upper and lower limb, loss of speech.
More here: https://ashfaqtaj098.blogspot.com/2021/02/60-year-old-male-patient-with-hrref.html?m=1
Case presentation links:
https://youtu.be/7rnTdy9ktQw
a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation:
A 60 year old man with a history of CVA 6 months back presented with
Dyspnea since 2 months
Bilateral pedal edema since 2 months
Reduced urine output since 2 months
Generalised weakness since 2 months
His Ecg shows poor R wave progression
Chest Xray PA shows Cardiomegaly
His 2Echo is suggestive of Heart failure DCMP with Hypokinesia at RCA, LCX
Anatomical diagnosis:
Coronary artery disease secondary to atherosclerosis
Risk factors:
Alcohol
Older Age
Male gender
2) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
Etiology to his current problems :
CAD leading to HFREF
Diagnosis:
DCMP with an EF of 34% secondary to CAD
CVA 6 months back (? Left ischaemic CVA) .
SEQUENCE OF EVENTS :
C) What is the efficacy of each of the drugs listed in his current treatment plan ?
A) Patient was put on
1) Salt and fluid restriction - which decreases pre load .
2) ACE/ARB - ACEi improves heart failure by decreasing afterload. Apart from decreasing the afterload, it also reduces cardiac myocyte hypertrophy. The Heart Outcomes Prevention Evaluation (HOPE) Study demonstrated better outcomes for those prescribed ACE inhibitors.
3) BETA BLOCKERS - Decreases heart rate and oxygen consumption and reduces angina. Prevent cardiac remodelling. Has survival benefit.
4) Diuretics - To reduce pre load on heart and also to prevent pulmonary edema.
A) SPIRINOLACTONE
P - In a doubleblind study, we enrolled 1663 patients who had severe heart failure and a left ventricular ejection fraction of no more than 35 percent and who were being treated with an angiotensin-converting-enzyme inhibitor, a loop diuretic, and in most cases digoxin.
I - total of 822 patients were randomly assigned to receive 25 mg of spironolactone daily
C - 841 to receive placebo
O -
The trial was discontinued early, after a mean follow-up period of 24 months, because an interim analysis determined that spironolactone was efficacious. There were 386 deaths in the placebo group (46 percent) and 284 in the spironolactone group (35 percent).
This 30 percent reduction in the risk of death among patients in the spironolactone group was attributed to a lower risk of both death from progressive heart failure and sudden death from cardiac causes. The frequency of hospitalization for worsening heart failure was 35 percent lower in the spironolactone group than in the placebo group.
B) ACE /ARB IN HEART FAILURE:
ACE-inhibitors improve symptoms and prognosis in patients with heart failure.
Besides sustained arterial and venous vasodilation the inhibition of the neurohumoral axis is thought to play an important role. Angiotensin II and catecholamines not only exert vasoconstrictor effects, but might also contribute to vascular and myocardial growth.
There is evidence that improvement of endothelial function might be involved in this effect, i.e., by reducing the degradation of bradykinin, an endothelial vasodilator. ACE inhibitors reduce LV hypertrophy, an important risk factor for cardiovascular disease and prognosis.
3) 52 year old male , shopkeeper by profession complains of SOB, cough ,decrease sleep and appetite since 10 days and developed severe hyponatremia soon after admission.
Case presentation video:
https://youtu.be/40OoVEQBgS4
a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation:
A 52 year old man, who is a known to be a Diabetic and hypertensive presented with:
Dyspnea since 10 days
Productive cough since 2 days
Disturbed sleep since 10 days
Anatomical localization:
The anatomical location of the problem is in the lungs
? Lower respiratory tract infection - but chestxray appears to be normal.
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
- Hyponatremia
-Lower respiratory tract infection
-Uncontrolled blood sugars
-Dimorphic Anemia
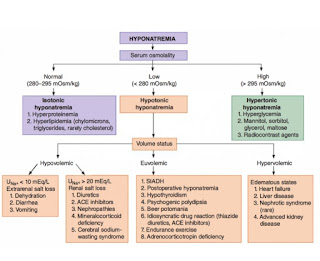
Pt could be having either hypervolemic hyponatremia secondary to heart failure.
Or euvolemic hyponatremia secondary to SIADH.
Intially due to uncontrolled sugars - Pseudo -hyponatremia was thought.( Translational hyponatremia)
APPROACH TO HYPONATREMIA:
C) What is the efficacy of each of the drugs listed in his current treatment plan especially for his hyponatremia? What is the efficacy of Vaptans over placebo? Can one give both 3% sodium as well as vaptan to the same patient ?
A) Randomized, double blinded, placebo-controlled trial to evaluate the efficacy and safety of tolvaptan in Chinese patients with hyponatremia caused by SIADH
To study the effect of tolvaptan on non-acute, non-hypovolemic hyponatremia in inappropriate secretion of antidiuretic hormone (SIADH) syndrome in Chinese patients. Hyponatremic SIADH patients received placebo (N = 18) or tolvaptan (N = 19) at an initial dose of 15 mg/day with further titration to 30 mg/day and 60 mg/day based on serum sodium concentrations. Randomized, double-blind, placebo-controlled trial. Primary endpoint was the change of the serum sodium from baseline to days 4 and 7.
The most common adverse events occurring in the tolvaptan group were dry mouth and thirst. Tolvaptan demonstrated superiority to placebo in the treatment of Chinese SIADH patients with hyponatremia by elevating serum sodium concentration with acceptable safety profile.
Tolvaptan and 3% NACL is not recommended to give together as there can be rapid correction of sodium more than 8-10 meq in 24 hrs.
That can lead to pontine myelinolysis.
4)Please mention your individual learning experiences from this month.
I was posted in nephrology in month of February.
Attended daily rounds and casualty cases.
Did workup for a long distance patient admitted for renal transplant.
Procedural competency - central venous lines and intubations.










Comments
Post a Comment