BIMONTHLY ASSESSMENT
This is an online assessment - BIMONTHLY
Link to above assesment:
https://medicinedepartment.blogspot.com/2020/12/medicine-question-paper-for-december.html?m=1
1) Link to the first question : 55 M with recurrent seizures.
https://ushaindurthi.blogspot.com/2020/11/55-year-old-male-with-complaints-of.html?m=1
A) Problem representation of the patient :
Ans) Recurrent Focal seizures(secondary to CVA)
Right hemiparesis with acute ischemic infarct in left fronto parietal area
Right multiple chronic infarcts
Uncontrolled sugars
Uncontrolled hypertension
Cause for CVA - ?Artero embolic stroke ( secondary to rupture of atherosclerotic plaque in vertebral or carotid artery)
Atherosclerosis bcoz of uncontrolled diabetic and hypertension.
Ecg is showing strain pattern and LVH .
I don't agree with the diagnosis of NSTEMI ,as subsequent ecgs were not showing any ST depressions or q waves .
So the source of embolism could be other factors than cardio embolic stroke.
Pt echo not showing any valvular heart disease or dilated chambers.
Anatomical site of leisons - Left frontal and parietal region .
B) Why are subcortical internal capsule infarcts more common than cortical infarcts ?
Ans) As lacunar vessels which supply internal capsule have smaller diameter,hence easily occluded.
Cerebrovascular accidents are more common in subcortical areas because the perforating arteries that supply the region are predisposed to occlusion or rupture due to their small diameter.
Ischemic strokes secondary to blockage of the perforating arteries are known as lacunar strokes.
The mechanisms of lacunar strokes include
1. Lipohyalinosis of perforating blood vessels - Most common cause
2. Atherosclerosis of the large trunk vessels that supply perforators
3. Embolic occlusion of the perforating arteries.
https://www.ncbi.nlm.nih.gov/books/NBK542181/
C) Pathogenesis of cortical infarct seizures :
Ans ) Stroke is most common cause of seizures.
Seizures mostly seem following hemorrhagic stroke than ischemic stroke.
Post stroke ----Early seizures - occur Less than 2 weeks of presentation of stroke.
Late seizures - >2 weeks after presentation of stroke
Post stroke :
Acute ischemic injury -- Accumulation of calcium and sodium resulting in depolarization of trans membrane potential and other Ca mediated effects.
|
It decreases seizures threshold .
- Glutamate excito toxicity
- Regional metabolic dysfunction
- So altered membrane potential and increased excitability and decreased threshold for seizures,
Remains major pathophysiology behind post stroke seizures.
- Ischemic penumbra - Region of viable tissue adjacent to infarcted core in ischemic stroke , contains electrically irritable tissue which is a focus for seizure.
- Global hypoperfusion can also cause seizures.
Hypoxic ischemic encephalopathy is most Como cause of status epilepticus.
LATE ONSET SEIZURES :
Associated with Persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause.
Risk of post Stroke seizures seen in :
ISCHEMIC - a) Increased severity of intial neurological deficit.
b) Severity of persistent disability after stroke.
c) Involvement of multiple sites /large leisons/Cortical damage .
d) Hippocampus ( vulnerable to ischemic insult and epileptogenic area )
e) Embolic stroke
HEMORRHAGIC -
a) SAH - MCA artery aneurysm
b) Intra parenchymal hematoma
Several authors have questioned the association of seizures with cardioembolic events. Seizures at onset were not a criterion in a data bank study of the cardiac causes of stroke. Intuitively, there is no reason to suspect that cardioembolic lesions would be more likely than emboli from large-vessel sources to cause seizures, as cardiac and large-vessel emboli frequently involve lesions to distal cortical branches. The mechanism by which cortical emboli precipitate seizures is uncertain, but possibilities include depolarization within an ischemic penumbra, rapid reperfusion after the fragmentation and distal migration of the embolus, or a combination of both.
Link to above data :
https://jamanetwork.com/journals/jamaneurology/fullarticle/781335
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2585721/
D ) Ecg changes :
Intial ecg showing
- Narrow qrs complex tachycardia -sinus tachy
- Regular with Rate of - 150 bpm and LAD
- Vpc present
- Lvh - R wave in avl >12 mm( modified Cornell criteria )
- Strain pattern present with st depressions . It doesn't look like NSTEMI as no reciprocal changes present and also subsequent ecg no q,st depressions present.
- Rbbb pattern present ( rsr in lead v1 and slurred s waves in v5-v6)
So LAD +RBBB - indicates bifasicular block.
Criteria for a bifasicular block :
Bifascicular block is the combination of RBBB with either LAFB or LPFB.
Left axis deviation (usually between -45 and -90 degrees)
Small Q waves with tall R waves (= ‘qR complexes’) in leads I and aVL
Small R waves with deep S waves (= ‘rS complexes’) in leads II, III, aVF
QRS duration normal or slightly prolonged (80-110 ms)
Prolonged R wave peak time in aVL > 45 ms
Increased QRS voltage in the limb leads.
On starting enoxaparin :
Idea behind starting anti coagulation in acute ischemic stroke or MI is to prevent further thrombus on exposed ruptured atherosclerotic plaque.
In embolic strokes -- First there is rupture of atherosclerotic plaque on vessel wall ---Raw surface thrombus is formed ,and breaking of that thrombus leading to embolus or complete obstruction by thrombus leads to ischemia .
Efficacy of lmwh : FISS TRIS TRIAL -Double blinded RCT .
P- Patients with acute ischemic stroke(AIS) and large vessel occlusive disease (LVOD) are taken and looked for END (Early neurological deterioration) defined as ERIS ( Early recurrent ischemic stroke)and SICH ( Symptomatic intra cranial hemorrhage)
603 pts had AIS AND LAOD .
I- 183 treated with LMWH.
173 - Treated with aspirin.
Patients were randomly assigned to receive either subcutaneous LMWH or oral aspirin within 48 hours after stroke onset for 10 days, then all received aspirin once daily for 6 months.
C - Comparison between aspirin and lmwh .
O - Among 353 patients included in the study, END within the first 10 days occurred in 6.7% of LMWH-allocated patients (12 of 180 patients) compared with 13.9% of aspirin-allocated patients (24 of 173). Low-molecular-weight heparin was significantly associated with the reduction of END (absolute risk reduction, 7.2%; odds ratio [OR], 0.44; 95% CI, 0.21-0.92). When individual components of END were examined, LMWH was significantly associated with a lower frequency of stroke progression within the first 10 days compared with aspirin (5.0% [9 of 180] vs 12.7% [22 of 173]
For patients with acute ischemic stroke and LAOD, treatment with LMWH within 48 hours of stroke may reduce END during the first 10 days, mainly by preventing stroke progression. The similar rate of cerebral hemorrhage between LMWH and aspirin demonstrated that LMWH may be safely used in acute ischemic stroke.
E) Which AED would you prefer ?
Given the typical focal onset of poststroke seizures, first-line therapy options include carbamazepine and phenytoin sodium.
Fosphenytoin sodium is also a noteworthy option in stroke patients because of lesser cardiotoxicity than phenytoin. Benzodiazepines, particularly lorazepam, should be initially administered to the patient with ongoing seizures.
The newer antiepileptic drugs are being touted as first-line agents for elderly patients because of their effectiveness and favorable side-effect profiles.
Although many of the newer anticonvulsants, eg, topiramate and levetiracetam, have been studied as adjunctive agents for refractory partial seizures, in practice they are often used as monotherapy.
Gabapentin has been shown to be efficacious as monotherapy for partial epilepsy.
2) 55 yr old man with recurrent hypoglycemia
http://manojkumar1008.blogspot.com/2020/12/shortness-of-breath-with-high-sugars.html
A ) Problem representation :
55 yr old male came with hypoglycemic attack. Pt is obese and known diabetic and hypertensive since 10 yrs and also has metabolic syndrome .
As patient presented with sob and cough ( non productive) - could be because of minimal bilateral pleural effusion which is transudative due to hypo albunemia -- which is again secondary to some chronic disease .? CKD ( as pt is having Anemia ,hypoalbunemia and proteinuria also ) .
Pt might be having CKD ( Diabetic nephropathy) intial stages where creatinine is not that much raised .
An USG ABDOMEN would have helped in knowing kidney size and RPD changes .
Fundoscopy also tells about the end organ damages.
I wouldn't suspect infections as pt is not having fever , tachycardia , elevated tlc .
B) Cause of recurrent hypoglycemia :
Secondary to OHA and Renal failure.
As renal profile is deranged , OHA won't be excreted, so constantly releasing insulin
Insulin also won't be excreted --as renal parameters are derranged.
Albumin loss - Is clearly explained by the renal failure in this patient - with the significant spot pc ratio 3.91 and high serum creatinine 2.7mg/dl.
CKD may promote hypoglycemia through :
a) Altered clearance of glucose-lowering medications,
b) Decreased kidney gluconeogenesis, and
c) Blunted counter-regulatory response to hypoglycemia.
d) Decreased clearance of insulin.
Here is an prospective observational study of hypoglycemia among 105 individuals with type 2 diabetes treated with insulin or a sulfonylurea .
P - 81 participants with CKD, defined as eGFR<60 ml/min per 1.73 m2, and 24 control participants with eGFR≥60 ml/min per 1.73 m2 frequency-matched on age, duration of diabetes, hemoglobin A1c, and glucose-lowering medications.
I - Each participant wore a continuous glucose monitor for two 6-day periods. We examined rates of sustained level 1 hypoglycemia (<70 mg/dl) and level 2 hypoglycemia (<54 mg/dl) among participants with CKD. We then tested differences compared with control participants as well as a second control population (n=73) using Poisson and linear regression, adjusting for age, sex, and race.
C - Over 890 total days of continuous glucose monitoring, participants with CKD were observed to have 255 episodes of level 1 hypoglycemia, of which 68 episodes reached level 2 hypoglycemia. Median rate of hypoglycemic episodes was 5.3 (interquartile range, 0.0–11.7) per 30 days and mean time spent in hypoglycemia was 28 (SD 37) minutes per day.
O - Among people with type 2 diabetes and moderate to severe CKD, hypoglycemia was common, particularly with tighter glycemic control.
- Severe hypoglycemia is associated with increased risks of cardiovascular events and mortality , and asymptomatic hypoglycemia has been associated with systemic inflammation and oxidative stress .
- In the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, participants with type 2 diabetes assigned to an intensive glycemic target experienced higher rates of severe hypoglycemia and a higher mortality rate than those assigned to a conventional glycemic target .
The Continuous Glucose Monitoring to Assess Glycemia in CKD (CANDY) study was a prospective, observational, cohort study designed to examine hypoglycemia and glycemic variability and to evaluate the performance of biomarkers of mean glycemia among people with type 2 diabetes and moderate to severe CKD.
P - Patients with a clinical diagnosis of type 2 diabetes treated with sulfonylurea or insulin (agents known to cause hypoglycemia) were eligible.
We first recruited participants with moderate to severe CKD (eGFR of 6 to <60 ml/min per 1.73 m2). We then recruited CANDY control participants (with eGFR≥60 ml/min per 1.73 m2) from the same source population, frequency-matching on the distributions of age, duration of diabetes, hemoglobin A1c, and glucose-lowering medication use of participants with CKD.
Results
Participant Characteristics
The 81 analyzed participants with CKD had a mean (SD) age of 69 (10) years, diabetes duration of 20 (11) years, body mass index of 33.8 (5.7) kg/m2, eGFR of 38 (14) ml/min per 1.73 m2, and hemoglobin A1c of 7.7% (1.4%) (Table 1); 74% were white, 51% had a college education, 89% used insulin (mainly basal bolus regimens), 21% used sulfonylureas, and 36% used other glucose-lowering medications (mainly biguanides and GLP1 receptor agonists)
Over 890 total days of CGM, participants with CKD were observed to have 255 episodes of hypoglycemia, including 68 episodes of level 2 hypoglycemia.
https://cjasn.asnjournals.org/content/14/6/844
c) What is the cause for his Dyspnea? What is the reason for his albumin loss?
A) Reason for his dyspnea could be heart failure or bilateral plueral effusion secondary to hypoalbunemia.
Would like to do a 2d echo to rule out .
Significant proteinuira could be secondary to diabetic nephropathy. USG abdomen and fundoscopy can be helpful in diagnosis.
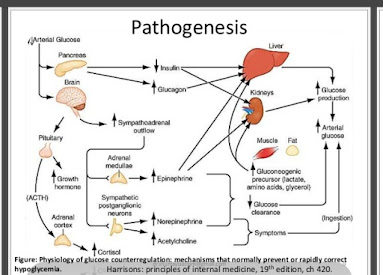
d) What is the pathogenesis involved in hypoglycemia ?
A)
Hypoglycemia is often defined by a plasma glucose concentration below 70 mg/dL; however, signs and symptoms may not occur until plasma glucose concentrations drop below 55 mg/dL
- WHIPPLE TRIAD - Symptoms of hypoglycemia, then obtain low blood glucose, and finally, demonstrate immediate relief of symptoms by the correction of the low blood glucose.
Physiological responses to decreased plasma glucose levels :
1) Decreased insulin - Primary glucose regulatory factor/ First defence against hypoglycemia.
2) Increased glucagon - Primary glucose counter regulatory factor / Second defence against hypoglycemia.
3) Increased epinephrine - Third defence, critical when glucagon is deficient.
4) Increased cortisol and growth harmone - Involved I'm defence against prolonged hypoglycemia. Not critical.
5) Symptoms - Prompt behavioural defence against hypoglycemia.
6) Decreased cognition- prevents behavioural defence against hypoglycemia.
- During fasting states, serum glucose levels are maintained via gluconeogenesis and glycogenolysis in the liver.
- Few major causes of hypoglycemia: pharmacologic, alcohol, critical illness, counter-regulatory hormone deficiencies, and non-islet cell tumors.
-Most cases of hypoglycemia occur in diabetic patients who are undergoing therapeutic intervention with meglitinides, sulfonylureas, or insulin. Drugs are the most common cause of hypoglycemia.
-Other potential causes of hypoglycemia are critical illness, alcohol, cortisol deficiency, or malnourishment.
-Alcohol inhibits gluconeogenesis in the body, but does not affect glycogenolysis.
- In critical illness states, for example, end-stage liver disease, sepsis, starvation, or renal failure, glucose utilization exceeds glucose intake, glycogenolysis and/or gluconeogenesis. The result of this imbalance is hypoglycemia.
-Counter-regulatory hormone deficiencies can occur as in states of adrenal insufficiency. Hypoglycemia associated with such deficiencies are rare.
-Non-islet cell tumors may also be a cause of hypoglycemia through increased secretion of insulin-like growth factor 2 (IGF-2).[2] IGF-2 increases glucose utilization, which can lead to hypoglycemia.
https://www.ncbi.nlm.nih.gov/books/NBK534841/
e) Do you agree with the treating team on starting the patient on antibiotics?
A) No, i do not agree with the treating team on starting the patient on antibiotics as patient has no fever , tachycardia and other signs of sepsis .Even cxr isn't showing any consolidation.
4) 75 year old woman with post operative hepatitis following blood transfusion
Case details here: https://bandaru17jyothsna.blogspot.com/2020/11/this-is-online-e-log-book-to-discuss.html
A)What are your differentials for this patient and how would you evaluate?
Ans ) This is a case of 75 F with mixed hyperbilirunenemia , pancytopenia , hepatitis ( elevated liver enzymes) , fever ,raised LDH.
All these features were acute onset indicating acute hemolytic reaction - most likely post transfusion related . As pt was normal previously.
So according to this flowchart , there is both elevated liver enzymes as well as bilirubin
So it comes under hepatocellular pattern, under which the differentials include ,
a) Viral etiology - Hepatitis A,B,C,D,E
b) Toxicity - Acetaminophen ,Drugs
c) Wilson's
d) Autoimmune hepatitis and.
e) Ischemic hepatitis
Most importantly patient is having Indirect coombs test postive .
- INDIRECT COOMBS TEST :
The indirect Coombs detects antibodies that are floating freely in the blood. These antibodies could act against certain red blood cells and the test can be done to diagnose reactions to a blood transfusion
The indirect Coombs test, also referred to as the indirect antiglobulin test (IAT), is used to detect in-vitro antibody-antigen reactions.
It is used to detect very low concentrations of antibodies present in a patient's plasma/serum prior to a blood transfusion.
In antenatal care, the IAT is used to screen pregnant women for antibodies that may cause hemolytic disease of the newborn
The Direct Coombs test detects antibodies that are stuck to the surface of the red blood cells.
https://en.m.wikipedia.org/wiki/Coombs_test
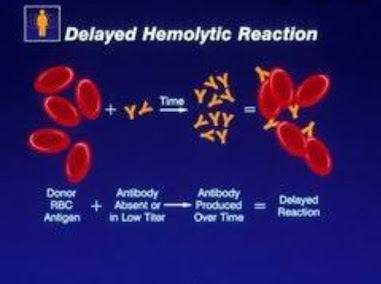
So considering this a delayed transfusion reaction is suspected with indirect hyperbilirunenemia and raised LDH , fever and hypotension .
Minimal amount of hypotension and stress leading to further deterioration of liver parameters - ? Ischemic hepatitis.
- Even hepatitis A or E can be suspected as acute infections ,but there are no symptoms of vomitings , diarrhoea , abdominal pain.
DELAYED TRANSFUSION REACTION :
- A delayed hemolytic transfusion reaction is a potentially significant adverse event caused by antibody mediated removal of recently transfused red cells due to an amnestic immune response from antibodies against an incompatible minor red blood cell antigen.
- This transfusion reaction can cause an unexpected drop in hemoglobin 3 - 28 days after a transfusion and can cause clinically observed symptoms, including fever
- Caused by an amnestic immune response, where red cell alloantibodies increase in titer and trigger removal of incompatible red cells via splenic macrophages.
- Diagnosis is supported by a new positive direct antiglobulin test (+IgG or +IgG and C3) and the detection of an alloantibody by antibody screen / panel or elution
Pathophysiology :
- Prior red cell exposure through pregnancy, transfusion or transplantation → sensitization to minor red blood cell antigens → primary immune response → alloantibody formation
- Commonly implicated minor antigens: Rh (D, C, c, E, e), Kidd (Jka, Jkb), Duffy (Fya, Fyb), Kell (K, k), MNS (M, N, S, s); antibodies are usually IgG reactive at 37°C and may or may not fix complement
- Commonly implicated minor antigens: Kidd antibodies (Jk) are most common and most severe
- Alloantibody titer decreases over time with no reexposure (transfusion / pregnancy) → pretransfusion testing becomes negative .
- Reexposure to antigens by offending transfusion / pregnancy → amnestic response → production of IgG → extravascular hemolysis
Clinical symptoms and laboratory findings (see below) typically occur 3 - 10 days (up to 28 days) after a transfusion of red blood cells that originally appeared compatible by testing
Patients have an unexpected drop in hemoglobin or less than expected rise in hemoglobin post transfusion
Delayed hemolytic transfusion reaction (DHTR) is typically mild but may necessitate additional transfusions.
https://www.pathologyoutlines.com/topic/transfusionmeddelayedtransfusionreaction.html
B) What would be your treatment approach? Do you agree with the treatment provided by the treating team and why? What are their efficacies?
A)
Specific intervention usually not indicated but symptomatic or supportive management can safely be used (i.e. antipyretics for fever).
Hydration and close monitoring are key for such cases.
Prevention is key:
- Accurate transfusion histories are critical to avoid delayed hemolytic transfusion reactions.
- Once a clinically significant alloantibody is identified, patient will receive red blood cell units that lack that antigen regardless of whether the antibody is detectable.
Supportive care is all that's needed. So the treating doctor has provided adequate hydration and maintained it .
Next question :
4) 60 year woman with Uncontrolled sugars
http://manojkumar1008.blogspot.com/2020/12/60-yr-old-female-with-uncontrolled.html
a) PROBLEM REPRESENTATION :
60 yr old female with chest pain : Differentials
A)
https://ebrary.net/27217/health/sepsis
https://jlb.onlinelibrary.wiley.com/doi/full/10.1189/jlb.0503195
c) Cxr findings :
A) Image quality : PA VIEW AND NO ROTATION
AIRWAY :
TRACHEA - CENTRAL
BRONCHI( RIGHT AND LEFT ) - NORMAL
ENLARGED HILAR LYMPHNODES
LUNG FILEDS :
RIGHT UPPER LOBE INCREASED OPACITY - CONSOLIDATION.
PLEURA - NO SIGNIFICANT ABNORMALITIES.
NO BLUNTING OF COSTO-PHRENIC ANGLES.
CARDIAC :
NORMAL HEART SIZE AND CARDIAC BORDERS VISIBLE.
Aortic knuckle visible .
DIAPHRAGM : NORMAL
NO BONY ABNORMALITIES.
NO TUBES ,DEVICES.
d) What do you think is the cause for her hypoalbuminaemia? How would you approach it?
A) Albumin is a negative phase reactant, hence is lowered in sepsis.
https://www.a4medicine.co.uk/hypoalbuminemia-low-albumin/#
E) Comment on the treatment given along with each of their efficacies with supportive evidence.
A) IV fluids and Insulin and other supportive care would be recommended.
Regarding the choice of antibiotics,ideal would be according to sputum culture sensitivity,
Initially monocef was started which was later escalated to piptaz and clarithromycin.
https://www.aafp.org/afp/2011/0601/p1299.html
As pt is admitted in ICU with comorbities - Choice would be beta lactam antibiotics plus a macrolide.
( Piptaz plus clarithromyci)
As Azithromycin has cardio toxicity risk.Its preferable to give clarithromycin.
Clinical Benefits of Piperacillin/Tazobactam versus a Combination of Ceftriaxone and Clindamycin in the Treatment of Early, Non-Ventilator, Hospital-Acquired Pneumonia in a Community-Based Hospital :
P -Retrospective cohort study was conducted in adult patients who were diagnosed with early, NV-HAP ( hosp acquired pneumonia)
Total of 89 patients were treated with ceftriaxone and clindamycin, while 124 received piperacillin/tazobactam. There were no significant differences between the two antibiotic groups with regard to median age, sex, or risk of pneumonia.
I -Patients were eligible for inclusion if they had received empiric treatment with either ceftriaxone and clindamycin or piperacillin/tazobactam for at least 3 days.
Results - The 30-day all-cause mortality did not differ significantly between the ceftriaxone plus clindamycin and piperacillin/tazobactam groups (4.5% vs 1.6%, P=0.202, respectively). However, in multivariate analysis, clinical failure was more frequent in the ceftriaxone plus clindamycin group than in the piperacillin/tazobactam group (HR 3.316; 95% CI, 1.589– 6918, P=0.001).
Conclusion: Treatment with piperacillin/tazobactam was more effective than that with ceftriaxone plus clindamycin in patients with early NV-HAP.
5) 56 year old man with Decompensated liver disease
Case report here: https://appalaaishwaryareddy.blogspot.com/2020/11/56year-old-male-with-decompensated.html
A ) What is the anatomical and pathological localization of the problem?
Liver - Chronic decompensated liver disease secondary to Hepatitis B .
Leading to complications like hypoalbunemia and third space loss with ascitis and Right massive pleural effusion.
Upper GI bleed and Portal hypertension.
Hematologic abnormalities - Anemia and thrombocytopenia with derranged coagulation profile.
Kidney- Acute kidney injury secondary to decreased perfusion to kidneys bcoz of third space loss.
Elevated serum creatinine and urea and hyperkalemia.
Also ? Hepato renal syndrome.
Abg showing metabolic acidosis.
B) How do you approach and evaluate this patient with Hepatitis B?
The 5 stages that have been identified in the viral life cycle of hepatitis B infection are briefly discussed below :
Stage 1: Immune tolerance
This stage, which lasts approximately 2-4 weeks in healthy adults, represents the incubation period. For newborns, the duration of this period is often decades. Active viral replication is known to continue despite little or no elevation in the aminotransferase levels and no symptoms of illnes
Stage 2: Immune active/immune clearance
In the immune active stage, also known as the immune clearance stage, an inflammatory reaction with a cytopathic effect occurs. HBeAg can be identified in the sera, and a decline in the levels of HBV DNA is seen in some patients who are clearing the infection. The duration of this stage for patients with acute infection is approximately 3-4 weeks (symptomatic period).
Stage 3: Inactive chronic infection
In the third stage, the inactive chronic infection stage, the host can target the infected hepatocytes and HBV. Viral replication is low or no longer measurable in the serum, and anti-HBe can be detected.
4: Chronic disease
The emergence of chronic HBeAg-negative disease can occur from the inactive chronic infection stage (stage 3) or directly from the immune active/clearance stage (stage 2).
Stage5: Recovery
In the fifth stage, the virus cannot be detected in the blood by DNA or HBsAg assays, and antibodies to various viral antigens have been produced. The image below depicts the serologic course of HBV infection.
https://www.researchgate.net/publication/281442059_A_Review_on_Therapeutic_Management_of_Chronic_Hepatitis_B_Infection
C) What is the pathogenesis of the illness due to Hepatitis B?
A) The life cycle of Hepatitis B virus is complex.
Attachment
The virus gains entry into the cell by binding to receptors on the surface of the cell and entering it by endocytosis mediated by either clathrin or caveolin-1.
Penetration
Following endocytosis, the virus membrane fuses with the host cell's membrane, releasing the nucleocapsid into the cytoplasm
Uncoating
Because the virus multiplies via RNA made by a host enzyme, the viral genomic DNA has to be transferred to the cell nucleus. It is thought the capsid is transported on the microtubules to the nuclear pore. The core proteins dissociate from the partially double stranded viral DNA, which is then made fully double stranded (by host DNA polymerases) and transformed into covalently closed circular DNA (cccDNA) that serves as a template for transcription of four viral mRNAs.
Replication
The largest mRNA, (which is longer than the viral genome), is used to make the new copies of the genome and to make the capsid core protein and the viral RNA-dependent-DNA-polymerase.
Assembly
These four viral transcripts undergo additional processing and go on to form progeny virions which are released from the cell or returned to the nucleus and re-cycled to produce even more copies.
Release
The long mRNA is then transported back to the cytoplasm where the virion P protein synthesizes DNA via its reverse transcriptase activity.
https://en.m.wikipedia.org/wiki/Hepatitis_B_virus
D. Is it necessary to have a separate haemodialysis set up for hepatits B patients and why?
- A) Patients undergoing dialysis treatment, and in particular hemodialysis (HD), are at increased risk for contracting viral infections
- This is due to their underlying impaired cellular immunity, which increases their susceptibility to infection.
- In addition, the process of HD requires blood exposure to infectious materials through the extracorporeal circulation for a prolonged period.
- Moreover, HD patients may require blood transfusion, frequent hospitalizations and surgery, which increase opportunities for nosocomial infection exposure.
- The most frequent viral infections encountered in HD units are hepatitis B (HBV), hepatitis C (HCV) and, to a lesser extent, human immunodeficiency virus infection (HIV).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4936461/
E) What are the efficacies of each treatment given to this patient? Describe the efficacies with supportive RCT evidence.
A) Efficacy Comparison of Tenofovir and Entecavir in HBeAg-Positive Chronic Hepatitis B Patients with High HBV DNA :
RETROSPECTIVE COHORT STUDY
P - A total of 96 HBeAg positive CHB patients were assessed, including 66 and 30 cases treated orally with entecavir at 0.5 mg/day (ETV group) and tenofovir at 300 mg/day (TDF group.
They were and years old in the ETV and TDF groups, respectively. No statistically significant differences were observed between the ETV and TDF groups patients in age, gender, height, weight, smoking and drinking history, HBV family history, baseline ALT levels, and HBV-DNA levels.
O- Patients treated with ETV and TDF had high viral response rates at 48 weeks (86.4% versus 96.7%), with a higher value in the TDF group, although the difference was not statistically significant (). At 36 w, the response rate in the TDF group was significantly higher than that obtained for ETV treated patients (90% versus 69.7%, p=0.03).
This study indicated that ETV and TDF have comparable efficacy in suppressing HBV-DNA replication and are well tolerated in HBeAg-positive nucleos(t)ide-naïve CHB patients with high HBV DNA.
https://www.hindawi.com/journals/bmri/2016/6725073/
6) 58 year old man with Dementia
Case report details: http://jabeenahmed300.blogspot.com/2020/12/this-is-online-e-log-book-to-discuss.html
1. What is the problem representation of this patient?
A) 58 year old man with Slurring of speech since 6 months
Drooling of saliva and food from the mouth since 6 months
Urinary incontinence since 6 months
Forgetfulness since 3 months
Dysphagia to both solids and liquids since 10 days
History of CVA 3 yrs ago and occasional alcholic.
2)How would you evaluate further this patient with Dementia?
A)
https://www.aafp.org/afp/2011/1015/p895.html
3) Do you think his dementia could be explained by chronic infarcts?
A)
Dementia is chronic, global, usually irreversible deterioration of cognition.
Vascular dementia is the 2nd most common cause of dementia among older people. It is more common among men and usually begins after age 70. It occurs more often in people who have vascular risk factors (eg, hypertension, diabetes mellitus, hyperlipidemia, smoking) and in those who have had several strokes.
Many people have both vascular dementia and Alzheimer disease.
Symptoms and signs of vascular dementia are similar to those of other dementias (eg, memory loss, impaired executive function, difficulty initiating actions or tasks, slowed thinking, personality and mood changes, language deficits).
However, compared with Alzheimer disease, vascular dementia tends to cause memory loss later and to affect executive function earlier.
Also, symptoms can vary depending on where the infarcts occur.
Unlike other dementias, multiple-infarct dementia tends to progress in discrete steps; each episode is accompanied by intellectual decline, sometimes followed by modest recovery.
https://www.msdmanuals.com/professional/neurologic-disorders/delirium-and-dementia/vascular-dementia
4) What is the likely pathogenesis of this patient's dementia?
A) https://www.frontiersin.org/articles/10.3389/fnagi.2013.00017/full
As compared with other conventional acetylcholinesterase inhibitors (AChEIs), donepezil is a highly selective and reversible piperidine derivative with AChEI activity that exhibits the best pharmacological profile in terms of cognitive improvement, responders rate (40%–58%), dropout cases (5%–13%), and side-effects (6%–13%) in AD.
P - The trial was of a multicenter, double-blind, parallel-group design and patients were randomised to once-daily treatment with either donepezil (1, 3 or 5 mg) or placebo. The 12-week double-blind phase was followed by a 2-week single-blind placebo washout. 161 patients (55-85 years of age) entered the study and 141 completed treatment.
I- DONEPEZIL 5MG OD
O- Patients treated with donepezil showed dose-related improvements in the Alzheimer''s Disease Assessment Scale - cognitive subscale score (ADAS-cog) and in MMSE scores.
The improvements in ADAS-cog were statistically significantly greater with donepezil 5 mg/day than with placebo.
There was a 50% reduction in the percentage of patients showing clinical decline with donepezil at 5 mg/day (11%) relative to placebo (20%).
https://www.karger.com/Article/Abstract/106895
7)
22 year old man with seizures
Case report here http://geethagugloth.blogspot.com/2020/12/a-22-year-old-with-seizures.html
1. What is the problem representation of this patient ? What is the anatomic and pathologic localization in view of the clinical and radiological findings?
A)
22 yr old male with
Headache since 2 months in occipital area radiating to frontal region.
Tonic seizures involving bilateral upper and lower limbs.
Fever low grade and weight loss and lymphadenopathy.
RVD POSITIVE
Alcoholic and smoker.
Ring enhancing leisons in right cerebellum
Anatomical localization - Brain ( Cerebellum)
2) . What the your differentials to his ring enhancing lesions?
A)
3) What is "immune reconstitution inflammatory syndrome IRIS and how was this patient's treatment modified to avoid the possibility of his developing it?
A )
A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating antiretroviral therapy in HIV-infected patients is defined as immune reconstitution inflammatory syndrome (IRIS).
- Current theories concerning the pathogenesis of the syndrome involve a combination of
(1) underlying antigenic burden,
(2) degree of immune restoration following Highly active antiretroviral therapy (HAART), and
(3) host genetic susceptibility
Whether elicited by an infectious or noninfectious agent, the presence of an antigenic stimulus for development of the syndrome appears necessary. This antigenic stimulus can be intact, “clinically silent” organisms or dead or dying organisms and their residual antigens. IRIS that occurs as a result of “unmasking” of clinically silent infection is characterized by atypical exuberant inflammation and/or an accelerated clinical presentation suggesting a restoration of antigen-specific immunity.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3221202/
https://medsphere.wordpress.com/2018/07/21/iris/amp/
3)41 year old man with Polyarthralgia
Case details here: https://mahathireddybandari.blogspot.com/2020/11/41m-with-chest-pain-and-joint-pains.html?m=1
a) 1. How would you evaluate further this patient with Polyarthralgia?
A)
2) Pathogenesis of rheumatoid arthritis ?
A)
8) MY LEARNING EXPERIENCES :
I was posted for my peripheral posting in cardiology from December first.
1/12/20- Submitted my postings letter to Principal and HOD of cardiology department and had to do few paper work.
Then Reported to opd .Sir posted me in opd for 1 week .So I was looking at the opd patients and learned 2d echo basics .
2/12/20 - Attended a case in emd . 60 yr old male came with complaints of chest pain since 8 hrs .Got diagnosed ad AWMI . Pt was started on heparin and nicorandil infusion and was shifted for angiogram and PTCA was done to LAD.
Read about ecg changes in AWMI and vessel occlusion.
3/12/20 - Followed cases in opd .Post PTCA patients and heart failure chronic management.
4/12/20 - Attended morning rounds in ICU .
Read about Heart failure pathophysiology and followed up cases in opd
5/12/20 - Attended morning rounds in ICU.
Did few bed side 2d echos . Read about basics of 2decho
6//12/20 - Sunday holiday . Read about ecg
changes in tachyarrythmias.
7/12/20 - As one week was over ,i was Posted in Cardiac ICU , for the next one week .
Attended morning rounds . Sir asked about reperfusion changes in ST ELEVATION MI.
So shared an article regarding it and read about it.
8/12/20 - Attended morning rounds in ICU.
55 yr old male who got admitted previous night for AWMI and was on inotropes , collapsed
So CPR was initiated ,pt developed VT , I gave DC shock ( Defibrillator) 200J ,but still patient couldn't be revived.
9/12/20 - Attended morning rounds in ICU.
Did bedside 2d echos , but couldn't get proper short axis and four chamber views .Need more practice and learning .
Saw aniogram procedures .Learned about coronary circulation.
10/12/20 - Applied leave due to family emergency.
11/12/20 - Attended morning rounds in ICU.
Typed few dischages and followed up investigations of the IP patients.
Read about Ticagrelor drug as many of the patients were being prescribed here 90mg stat dose of ticagrelor prior to PTCA .
12/12/20 - Attended morning rounds in ICU.
Attended opd for few hours , Sir asked to identify a tachyarrythmia ecg . I could get it as atrial tachycardia but it even had 2:1 block.
So read few points about that ecg.
13/12/20 - Sunday holiday.
14/12/20 - Attended morning rounds in ICU.
Attended few cross consultations for fitness and hypertension.
Saw temporary pace maker procedure.
Read about tirofiban drug.
Monitoring of pts in ICU .
15/12/20 - Attended morning rounds in ICU.
Read about Heparin drug ,as all MI pts were being started on heparin infusion here.
16/12/20 - Attended morning rounds in ICU.
Attended Emd calls .
50 yr old female with extensive AWMI was unstable and had pulmonary odema .So was started on CPAP .
She developed heart block and a temporary pacing was done.
17/12/20 - Attended morning rounds in ICU.
75 yr old male was admitted AWMI with qrbbb ,he had severe lv dysfunction on echo and was put on inotropes .
That patient heart rate starting dropping suddenly ,so i took an ecg which showed complete heart block. I gave 1mg atropine , but there was no response ,so in informed sir ,pt was shifted immediately
for temporary pace maker placement.
18/12/20 - Attended morning rounds in ICU.
Followed up discharges . Read about ecg changes in different types of heart block.
19/12/20 - Attended morning rounds in ICU.
Saw an interesting case got admitted last night , 20 yr old male with AWMI .
He was having accelerated idioventricular rythm in morning ecg .
He has a family history of young onset MI,he was planned for angio today.
Have to evaluate further for young onsent MI.















































Comments
Post a Comment