CUSHINGS SYNDROME -
19 year old male resident of Nalgonda and currently studying intermediate ,came to opd with complaints of :
-Itchy Ring leisons over arms ,abdomen ,thigh and groin since 1 and half year .
-Purple stretch marks all over abdomen ,lower back ,upper limbs ,thighs since 1 year .
-Abdominal distension and facial puffiness since 6 months.
- Pedal edema since 3 months.
- Low back ache since 3 months .
- Feeling low , not feeling to talk to anyone.
- Weight gain and decreased libido since 3months.
- Loss of libido and erectile dysfunction since 2 months .
Pt was apparently alright one and half year ago , when he slowly developed erythematous round leisons which are annular shaped and itchy all over abdomen , upper limb ,groin and inner thigh region .
No history of fever back then. No other complaints apart from skin lesions.
Pt visited local RMP where he prescribed auyurvedic medications and other creams ( unknown composition as pt don't have them currently ). He also prescribed tablets (unknown composition) . Patient started using all these medications for 1-2 months .
Leisons reduced a bit after using medications .
Later after 2 months he developed multiple hyper pigmented plaques over lower limbs ,abdomen , for which he again visited same place and used ayurvedic oils over the leisons.
He also used clobetasol ointment over the leisons.(for approximately 1 year all over the body)
He started noticing pink striae over his abdomen first 1 year ago and later on back and over arms,which were gradually increasing in size .
Later he visited a hospital and used miconazole and luliconazole ointments also.
He used clobetasol ointment all over the leisons for long time .
He started noticing abdominal distension and facial puffiness ,weight gain, but never visited any hospital.
Later he developed pedal edema and low back ache since 3 months .
His consulted a dermatologist at this point of time who advised to consult physician and prescribed monteleukast , itraconazole tablets ,luliconazole ointment for tenia corporis.
He stopped all medications one month ago and visited our opd with complaints of pink striae and easy fatigue ,weakness and low back ache .
His brother also gave history of pt being moody and feeling of low self esteem due to multiple leisons.
He even complaints pt wouldn't step out of house and always stays indoor and wouldn't interact with others .
No complaints of chest pain ,sob , palpitations .
No complaints of decreased or frothy urine.
No other negative history.
No h/o DM,HTN,TB,ASTHMA,CAD.
ALLERGIC HISTORY - pt gives h/o allergy to eggs ,brinjal .
O/E : Pt was c/c/c
BP - 160/100 mmHg
Pr - 96 BPM ,regular ,normovolemic .
Rr - 18/min
Spo2- 98% on ra.
Weight - 63 kg.
Height - 175 cm.
GENERAL EXAMINATION :
NO pallor ,icterus ,cyanosis , clubbing, lymphadenopathy.
Pedal edema present - pitting type extending upto knee.
Abdominal distension present.
Moon face present
Pink striae noted over anterior abdominal wall and on low back and on upper arms and thighs.
Thin skin present .
Poor healing noticed over leg ulcers and easy bruising noted .
Acne present over face .
Acanthosis nigrans noted over neck.
GYNECOMASTIA PRESENT .
neck pad of fat present .
Sparse scalp hair .
.
Skin examination - Multiple itchy erythematous annular leisons noted all over abdomen , upper limb ,groin and inner thigh region .
Multiple hyperpigmented plaques noted over bilateral lower limbs .
SYSTEMIC EXAMINATION :
CVS - S1S2 heard .No murmurs
RS - BAE present .
No adventitious sounds .
P/A - Soft , distended .
No organomegaly .
Bowel sounds present .
CNS - HMF - INTACT R. L
MOTOR SYSTEM - POWER - UL 5/5 5/5
LL 5/5 5/5
Proximal muscles lower limb - power is 4/5 .
TONE - NORMAL.
REFLEXES - B. T. S. K. A. P
R. +2 +2. +1. +2. +1. FELXOR
L. +2. +2. +2. +2. +1. FLEXOR.
CRANIAL NERVES - NORMAL .
Difficulty in getting up from chair was noticed.
PROVISIONAL DIAGNOSIS -
? IATROGENIC CUSHINGS SYNDROME .
TINEA CORPORIS .
DENOVO HTN .
INVESTIGATIONS :
CBP - HB - 13.4 g/dl
TLC - 6,800
PLT - 1.5 lakhs.
RBS - 139 mg/dl
CUE - ALBUMIN - +1
SUGARS - NIL .
PUS CELLS - 3-4
RBC - NIL .
LFT - TB -1.03
DB-0.21
ALBUMIN - 3.9
RFT - UREA - 22
SERUM CREATININE -0.6
ELECTROLYTES - NA - 136
K- 4
CL-98
USG ABDOMEN - NORMAL.
ECG - SINUS TACHYCARDIA
LVH PRESENT.
This was picture of striae one year ago when it gradually started :
On presentation to opd pictures : 28/05/21
We took dermatologist opinion for tenia corporis where they advised
Ointment AMLORFINE
FUSIDIC ACID CREAM.
SALINE COMPRESS OVER LEISONS.
Plan to start anti fungals on next visit once dose of steroids is reduced .
OPTHAL opinion Was taken to look for visual acuity and cataract .
No features of lens opacities noted .
BUT IOP was high ,where they advised to follow up .
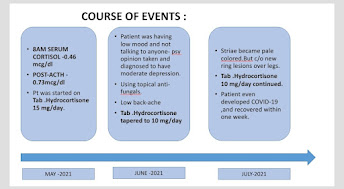
We advised pt to get fasting 8am serum cortisol levels and was planned to start on low dose steroids to avoid adrenal crisis.
8AM S CORTISOL LEVELS (30/5/21)
- 0.46 mcg/dl ( very low) .
( normal range - 4.3-22.4 mcg/dl).
In view of lvh pt was started on tab telma 20 mg od .
On 3/6/21 - ACTH STIMULATION TEST WAS DONE .
BY INJECTING 0.4 ML OF ACTOM PROLONGATUM INJECTION (ACTH) INTRA MUSCULAR @ 7am
1 HR LATER FASTING SERUM CORTISOL SAMPLE WAS SENT .
VALUE - 0.73 mcg/dl
Indicating there was HPA AXIS suppression and pt was started on TAB HIZONE 15 mg per day in three divided doses @ 8am ,12 pm and 4 pm.
Pt was asked to follow up after one month .
FINAL DIAGNOSIS :
IATROGENIC CUSHINGS SYNDROME SECONDARY TO TOPICAL CLOBETASOL APPLICATION ALL OVER BODY FOR APPROXIMATELY ONE YEAR.
TINEA CORPORIS
DENOVO HTN .
FOLLOW UP -
ON NEXT VISIT : ( 25/6/21).
Pt was symptomatically better , pedal edema subsided.
Striae were pale in color and we're subsiding.
Weight - 67kg
Ht -175 cm.
Bp- 160/100 mmHg.
Pr -88bpm.
Dose of Tab hizone was reduced to 10 mg per day in divided doses for one month.
In view of low back ache Xray LS spine was done which was normal and pt was advised.:
Tab Shelcal 500 OD and Tab Vit D 3 Od.
Tab ULTRACET /PO/SOS.
Psychiatry opinion was taken and he was diagnosed with moderate depression .
In July 2021 pt was complaining of fever ,sore throat and dry cough since 3 days and he was tested positive for COVID 19 , we advised him home isolation and PCM 650 Mg /po /tid x 5 days .
He was advised to continue tab hizone tablets as it was advised. ( 10mg/day in divided doses.)
-INJ HYDROCORTISONE 100mg sos if pt is in adrenal shock.
He recovered from COVID within one week .
Next visit : ( 6/8/21).
BP- 170/100 - TELMA DOSE WAS INCREASED TO 40 MG OD.
PR - 88bpm.regular , normovolemic.
Wt- 69 kg
Height -
Abdominal girth - 96cm
Pt complaints of excoriation over striae and appearance of erythematous macules over abdomen whenever he takes food he is allergic to.
Took dermatologist opinion for it . They started him on Tab Itraconazole 100 mg bd for 2 weeks. And lulifin cream and tab levocitrixine 5mg od.
His brother complaints of depressed mood , pt not going out due to social stigma. Psychiatric counselling was given .
He still complaints of low back ache..othropedics opinion was taken and advised to continue Ultracet and tab Shelcal .
Cbp , cue and electoltes were repeated which were all in normal range .
USG ABDOMEN was done - Normal kidney size bilateral and CMD maintained. No other sonological abnormality noted.
As his lesions dint subside we reduced dose of hisone to 7.5 mg per day ,to see response.
Review psychiatry and opthal opinion was taken , where his lens was clear - no e/o cataract .
no retinopathy changes and no raised IOP and his visual acuity was 6/6.
0N 20/8/21 - IN view of constant low back ache , MRI LS SPINE WAS done with whole soine screening .
which showed lumbar epidural lipomatosis .
Mild depression of superior endplates of D12 and L4 - Likely subacute /chronic compression .
L3-L4 disc degeneration with mild diffuse disc bulge causing no significant neural foramen stenosis .
ON 24/8/21 - Pt developed painful swelling and redness of right lower limb along with intermittent fever - DIAGNOSED TO HAVE RIGHT LOWE LIMB CELLULITIS .
Pt was admitted and was given IV AUGMENTIN for 5 days and MGSO4 dressings were done .
TAB chymerol forte was given for 5 days.
Tab hisone 7.5 mg was continued in divided doses .
-INJ HYDROCORTISONE 100mg sos if pt is in adrenal shock.
PT again came for follow up in september , complaints of weight gain , but striae reduced and patient attender was giving history of patient having low mood and constantly being at home and not doing any exercise .
He was having social inhibition and was avoiding contact with other people.
We sent him for psychiatry where brief counselling was given .
TAB HISONE dose was reduced to 5 mg /day.
Next follow up was in october (22/10/11) ,pt improved and dose was further reduced to 2.5 mg/day .
PT again visited to our OPD on 23/ 11/21 , again with
c/o increasing striae and abdominal distension.since one month .( Striae were same as before ,but pt was feeling that way )
Abdominal distension could be due to fat accumulation,as pt was hardly exercising and is only staying at home and eating food.
weight gain present .( 76kg ).
c/o diminished vision
BP-160/100 mmhg
PR - 110 bpm
CVS- S1 S2 PRESENT
RS - BAE present and clear .
Pt was giving history of good compliance to medications and was using tab hisone 2.5mg only since past one month .No history of other medications ( ayurvedic or homeopathic ) usuage .
He is still having social inhibiton and is not going out of house or doing regular exercise .
P is having lot of anxiety and psychiatric issues.
As his blood pressure is uncontrolled and ECG having LVH - we increased the dose of anti-htn to TAB TELMA AM 40/5 mg OD.
HIS ROUTINE investigations were repeated , cbp,s. electrolytes ,s.creat was normal .
HIS RBS was 178 mg/dl
HBA1C was 6.5 %
Review Dermat opinion was taken ,
PT dint use his cream and itraconazole tablets regularly last month .
Review psychiatry opinion taken - Adjustment issues due to underlying illness.
Brief psychotherapy given .
REVIEW ENDOCRINE OPINION TAKEN (26/11/21) : Pt apprehensive .
Stopped hisone 2.5 mg and observe patient.
Only stress dose - Inj hydrocortisone 100 mg IV IF PT IS IN Adrenal shock .
Adv -8am serum cortsiol

























































Comments
Post a Comment